Film coated tablets (10 mg), Oral Suspension (1 mg/ml)
COMPOSITION:
Each film-coated tablets contains: 10 mg Domperidone.
Each 5 mL of oral suspension contains: 5 mg Domperidone. Excipients:
Film-coated tablets:
Core: Lactose Monohydrate, Starch, Talc, Magnesium Stearate, Aerosil, Povidone, Deionized Water. Film: HPMC, Talc, PEG, Ethanol, Titanium Dioxide.
Oral suspension: CMC, Vivapor, Saccharin Sodium, Tween, Banana Flavor, Antifoam Emulsion, Sorbitol, Methyl Paraben Sodium, Propyl Paraben Sodium, Deionized Water.
Pharmacological classification: Antispasmodic drugs and antiemetic.
MECHANISM OF ACTION:
Domperidone is a dopamine antagonist with anti-emetic properties. Its anti-emetic effect may be due to a combination of peripheral effects and antagonism of dopamine receptors in the chemoreceptor trigger zone.
PHARMACOKINETICS:
Absorption: Domperidone is rapidly absorbed after oral administration, with peak plasma concentrations occurring at approximately 1 hr after dosing.
Distribution: Domperidone is 91-93% bound to plasma proteins.
Metabolism: Domperidone is metabolized by liver.
Excretion: 31% of the drug is excreted by urine and 66% is excreted by feces. INDICATIONS:
MOTALON is indicated for the relief of the symptoms of nausea and vomiting.
CONTRAINDICATIONS:
The drug is contraindicated in hypersensitivity to MOTALON or any of the excipients. Prolactin-releasing pituitary tumour. When stimulation of the gastric motility could be harmful e.g in patients with gastro- intestinal haemorrhage, mechanical obstruction or perforation. In patients with moderate or severe hepatic impairment. In patients who have known existing prolongation of cardiac conduction intervals, particularly QTc, patients with significant electrolyte disturbances or underlying cardiac diseases such as congestive heart failure. co-administration with QT-prolonging drugs.co-administration with potent CYP3A4 inhibitors (regardless of their QT prolonging effects).
ADVERSE EFFECTS:
The most common adverse reaction while taking the drug is dry mouth. The uncommon adverse effect: Loss of libido, Anxiety, Somnolence, Headache, Diarrhea, Rash, Pruritus, Galactorrhoea, Breast pain, Asthenia.
DRUG INTERACTIONS:
Concomitant use of the following substances is contraindicated:
QTc prolonging medicinal products such as, anti-arrhythmic class IA (e.g. disopyramide, hydroquinidine, quinidine), anti-arrhythmic class III (e.g. amiodarone, dofetilide, dronedarone, ibutilide, sotalol), certain anti- psychotics (e.g. haloperidol, pimozide, sertindole), certain anti-depressants (e.g. citalopram, escitalopram), certain antibiotics (e.g. erythromycin, levofloxacin, moxifloxacin, spiramycin), certain antifungal agents (e.g. pentamidine), certain antimalarial agents (in particular halofantrine, lumefantrine), certain gastro-intestinal medicines (e.g. cisapride, dolasetron, prucalopride), certain antihistaminics (e.g. mequitazine, mizolastine), certain medicines used in cancer (e.g. toremifene, vandetanib, vincamine), certain other medicines (e.g. bepridil, diphemanil, methadone), Potent CYP3A4 inhibitors i.e. (protease inhibitors, systemic) azole antifungals, some macrolides (erythromycin, clarithromycin, telithromycin).
Concomitant use of the following substances is not recommended: Moderate CYP3A4 inhibitors i.e. diltiazem, verapamil and some macrolides. Concomitant use of the following substances requires caution in use: caution with bradycardia as well as with the following macrolides involved in QT-interval prolongation: azithromycin and roxithromycin (clarithromycin is contra-indicated as it is a potent CYP3A4 inhibitor).
WARNINGS AND PRECAUTIONS:
Cardiovascular effects:
MOTALON has been associated with prolongation of the QT interval on the electrocardiogram. There have been very rare cases of QT prolongation and torsades de pointes in patients taking MOTALON. These reports included patients with confounding risk factors, electrolyte abnormalities and concomitant treatment. MOTALON was associated with an increased risk of serious ventricular arrhythmias or sudden cardiac death, a higher risk was observed in patients older than 60 years, patients taking daily doses greater than
30 mg, and patients concurrently taking QT-prolonging drugs or CYP3A4 inhibitors MOTALON should be used at the lowest effective dose in adults and children.
MOTALON is contraindicated in patients with known existing prolongation of cardiac conduction intervals, particularly QTc, in patients with significant electrolyte disturbances (hypokalemia, hyperkalemia,
hypomagnesaemia), or bradycardia, or in patients with underlying cardiac diseases such as congestive heart failure due to increased risk of ventricular arrhythmia.
Treatment with MOTALON should be stopped if signs or symptoms occur that may be associated with cardiac arrhythmia, and the patients should consult their physician.
Pregnancy and lactation:
MOTALON should only be used during pregnancy when justified by the anticipated therapeutic benefit. In breast-feeding mothers, a decision should be made whether to discontinue breast-feeding or to discontinue MOTALON therapy taking into account the benefit of breast-feeding for the child and the benefit of therapy for the woman. Caution should be exercised in case of QTc prolongation risk factors in breast-fed infants. MOTALON should be used at the lowest effective dose for the shortest duration necessary to control nausea and vomiting.
It is recommended to take oral MOTALON before meals. If taken after meals, absorption of the drug is somewhat delayed.
If a scheduled dose is missed, the missed dose should be omitted and the usual dosing schedule resumed. The dose should not be doubled to make up for a missed dose.
Usually, the maximum treatment duration should not exceed one week.
Adults and adolescents (12 years of age and older and weighing 35 kg or more):
One 10 mg tablet before meal up to three times per day with a maximum dose of 30 mg per day.
10 ml (of oral suspension containing domperidone 1 mg per mL) up to three times per day with a maximum daily dose of 30 ml per day.
*Due to the need for accurate dosing, the drug is unsuitable for use in children and adolescents weighing less than 35 kg.
Neonates, infants, children (less than 12 years of age) and adolescents weighing less than 35 kg:
MOTALON Tablets: the risk of neurological side effects is higher in young children. Overdosing may cause extrapyramidal symptoms in children.
MOTALON Suspention: The dose is 0.25 mg/kg. This should be given up to three times per day with a maximum dose of 0.75 mg/kg per day.
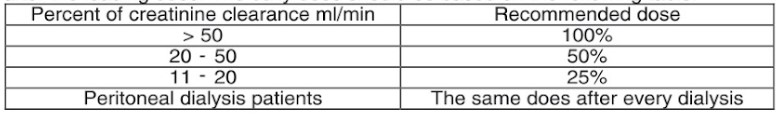
Renal impairment: The elimination half-life of MOTALON is prolonged in severe renal impairment. The dose may also need to be reduced.
Hepatic Impairment: MOTALON is contraindicated in moderate or severe hepatic impairment. Dose modification in mild hepatic impairment is however not needed
OVERDOSAGE:
Overdose has been reported primarily in infants and children. Symptoms of overdosage may include agitation, altered consciousness, convulsions, disorientation, somnolence and extrapyramidal reactions. Treatment: There is no specific antidote to MOTALON, but in the event of overdose, standard symptomatic treatment should be given immediately. Gastric lavage as well as the administration of activated charcoal, may be useful. ECG monitoring should be undertaken, because of the possibility of QT interval prolongation. Close medical supervision and supportive therapy is recommended. Anticholinergic, anti- parkinson drugs may be helpful in controlling the extrapyramidal reactions.
PACKAGING:
Film-coated tablets: 3 blisters, each contains 10 film-coated tablets/carton box.
Oral suspension: Glass bottle of 100 mL oral suspension/carton box, with a metallic screw cap. STORAGE CONDITIONS:
– Protect from light and moisture. – Store below 30°C.