Miconazole Nitrate 2% + Hydrocortisone (Acetate) 1%
Topical (Cream, Ointment)
COMPOSITION:
Each 100 g of MECOZALEN CORT (cream, ointment) contains: Miconazole nitrate 2g, Hydrocortisone (as Hydrocortisone acetate) 1 g.
EXCIPIENTS:
MECOZALEN CORT cream: Cetylstearyl Alcohol with Ethylene Oxide, Cetostearyl Alcohol, Liquid Paraffin, Benzoic Acid, Disodium Edetate, Butylated Hydroxyanisole, Sodium Hydroxide Solution, Purified Water.
MECOZALEN CORT ointment: Polyethylene, Liquid Paraffin gel.
INDICATIONS:
For the topical treatment of inflamed dermatosis where infection by susceptible organisms and inflammation co-exist, e.g. intertrigo and infected eczema.
Moist or dry eczema or dermatitis including atopic eczema, primary irritant or contact allergic eczema or seborrhoeic eczema including that associated with acne.
Intertriginous eczema including inflammatory intertrigo, perianal and genital dermatitis.
Organisms which are susceptible to miconazole are dermatophytes and pathogenic yeasts (e.g. Candida spp.). Also many Gram- positive bacteria including most strains of Streptococcus and Staphylococcus.
DOSAGE AND ADMINISTRATION:
For topical administration.
Apply MECOZALEN CORT two or three times a day to the affected area, rubbing in gently until it has been absorbed by the skin. Because of its corticosteroid content avoid long-term treatment with MECOZALEN CORT. Once the inflammatory symptoms have disappeared (after about 7 days),
treatment can be continued where necessary with MECOZALEN CORT (miconazole nitrate 2%). Treatment should be continued without interruption until the lesion has completely disappeared (usually after 2 to 5 weeks).
If after about 7 days’ application, no improvement has occurred, cultural isolation of the offending organism should be followed by appropriate local or systemic antimicrobial therapy.
The same dosage applies to both adults and children.
Elderly
Natural thinning of the skin occurs in the elderly, hence corticosteroids should be used sparingly and for short periods of time.
Pediatrics
In infants and children, caution is advised when MECOZALEN CORT is applied to extensive surface areas or under occlusive dressings including baby napkins (diapers). In infants, long term continuous topical corticosteroid therapy should be avoided. CONTRAINDICATIONS:
– True hypersensitivity to miconazole/miconazole nitrate, other imidazole derivatives, hydrocortisone or to any of the excipients. – Tubercular or viral infections of the skin or those caused by Gram-negative bacteria.
WARNINGS AND PRECAUTIONS:
– When MECOZALEN CORT is used by patients taking oral anticoagulants, the anticoagulant effect should be carefully monitored. Severe hypersensitivity reactions, including anaphylaxis and angioedema, have been reported during treatment with MECOZALEN CORT and with other miconazole topical formulations. If a reaction suggesting hypersensitivity or irritation should occur, the treatment should be discontinued.
– MECOZALEN CORT must not come into contact with the mucosa of the eyes.
– As with any topical corticosteroid, caution is advised with infants and children when MECOZALEN CORT is to be applied to extensive surface areas or under occlusive dressings including baby napkins; similarly, application to the face should be avoided. – In infants, long term continuous topical corticosteroid therapy should be avoided. Adrenal suppression can occur even without occlusion.
– Because of its corticosteroid content avoid long-term treatment with MECOZALEN CORT. Once the inflammatory symptoms have disappeared treatment may be continued with miconazole nitrate 2% cream or powder.
– MECOZALEN CORT can damage certain synthetic materials. Therefore, it is recommended to wear cotton underwear if this clothing comes into contact with the affected area.
– The concurrent use of latex condoms or diaphragms with vaginal anti-infective preparations may decrease the effectiveness of latex contraceptive agents. Therefore, MECOZALEN CORT should not be used concurrently with a latex condom or latex diaphragm. Visual disturbance
Visual disturbance may be reported with systemic and topical corticosteroid use. If a patient presents with symptoms such as blurred vision or other visual disturbances, the patient should be considered for referral to an ophthalmologist for evaluation of possible causes which may include cataract, glaucoma or rare diseases such as central serous chorioretinopathy (CSCR) which have been reported after use of systemic and topical corticosteroids.
INTERACTION:
Miconazole administered systemically is known to inhibit CYP3A4/2C9. Due to the limited systemic availability after topical application, clinically relevant interactions are rare. However, in patients on oral anticoagulants, such as warfarin, caution should be exercised and anticoagulant effect should be monitored.
Miconazole is a CYP3A4 inhibitor that can decrease the rate of metabolism of hydrocortisone. Serum concentrations of hydrocortisone may be higher with the use of MECOZALEN CORT compared with topical preparations containing hydrocortisone alone.
PREGNANCY:
Clinical data on the use of MECOZALEN CORT in pregnancy are limited. In animals, corticosteroids are known to cross the placenta and consequently can affect the fetus. Administration of corticosteroids to pregnant animals can cause abnormalities of fetal development. The relevance of these findings to humans has not been established.
As a precautionary measure, it is preferable to avoid the use of MECOZALEN CORT during pregnancy. Treatment of large surfaces and the application under occlusive dressing is not recommended.
BREAST-FEEDING
There are no adequate and well-controlled studies on the topical administration of MECOZALEN CORT during breastfeeding. It is not known whether concomitant topical administration of MECOZALEN CORT to the skin could result in sufficient systemic absorption to produce detectable quantities of hydrocortisone and miconazole in breast milk in humans. A risk to the newborn child cannot be excluded.
A decision must be made whether to discontinue breast-feeding or to discontinue/abstain from MECOZALEN CORT therapy taking into account the benefit of breast feeding for the child and the benefit of therapy for the woman. Treatment of large surfaces and the application under occlusive dressing is not recommended.
OVERDOSE:
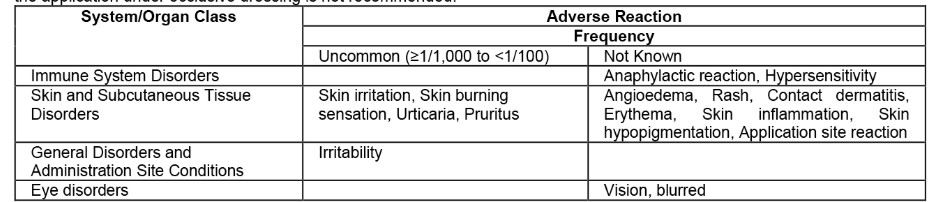
Adverse Reaction Frequency
Not Known
Anaphylactic reaction, Hypersensitivity Angioedema, Rash, Contact dermatitis, Erythema, Skin inflammation, Skin hypopigmentation, Application site reaction Vision, blurred Prolonged and excessive use can result in skin irritation, which usually disappears after discontinuation of therapy. Topically applied corticosteroids can be absorbed in sufficient amounts to produce systemic effects.
PHARMACOLOGICAL PROPERTIES:
Pharmacodynamic effects:
Miconazole nitrate is active against dermatophytes and pathogenic yeasts, and many Gram-positive bacteria. Hydrocortisone is an anti-inflammatory steroid. Its anti-inflammatory action is due to reduction in the vascular component of the inflammatory response, suppression of migration of polymorphonuclear leukocytes, and reversal of increased capillary permeability. The vasoconstrictor action of hydrocortisone may also contribute to its anti-inflammatory activity. Pharmacokinetic properties:
Absorption:
Miconazole remains in the skin after topical application for up to 4 days. Systemic absorption of miconazole is limited, with a bioavailability of less than 1% following topical application of miconazole. Plasma concentrations of miconazole and/or its metabolites were measurable 24 and 48 hours after application. Approximately 3% of the dose of hydrocortisone is absorbed after application on the skin.
Distribution:
Absorbed miconazole is bound to plasma proteins (88.2%) and red blood cells (10.6%). More than (90%) of hydrocortisone is bound to plasma proteins.
Metabolism and elimination:
The small amount of miconazole that is absorbed is eliminated predominantly in feces as both unchanged drug and metabolites over a four-day post-administration period. Smaller amounts of unchanged drug and metabolites also appear in urine.
The half-life of hydrocortisone is about 100 minutes. Metabolism takes place in the liver and tissues and the metabolites are excreted with the urine, mostly as glucuronides, together with a very small fraction of unchanged hydrocortisone. INCOMPATIBILITIES:
Contact should be avoided between latex products such as contraceptive diaphragms or condoms and MECOZALEN CORT since the constituents of MECOZALEN CORT may damage the latex.
STORAGE CONDITIONS:
“Store at room temperature, below 25 °C”.
“Do not freeze”.
“Keep out of reach of children”.
PRESENTATION:
Aluminium tube contains 15 gram MECOZALEN CORT cream.
Aluminium tube contains 15 gram MECOZALEN CORT ointment.