Excipients: Carboxymethyl Cellulose Sodium, Starch, Propylene Glycol, Saccharin Sodium, Strawberry Flavor, Tween, Deionized Water.
ACTIONS:
MECOZALEN possesses an antifungal activity against the common dermatophytes and yeasts as well as an antibacterial activity against certain gram-positive bacilli and cocci.
Its activity is based on the inhibition of the ergosterol biosynthesis in fungi and the change in the composition of the lipid components in the membrane, resulting in fungal cell necrosis.
PHARMACOKINETICS:
Absorption:
Oral bioavailability of MECOZALEN is low (25-30) % because of low gastrointestinal absorption.
Miconazole is systemically absorbed after administration as the oral gel. Administration of 60 mg dose of Miconazole Oral Gel results in peak plasma concentrations of 31-49 ng/mL, occurring approximately two hours post-dose. Distribution
Absorbed Miconazole is bound to plasma proteins (88.2%), primarily to serum albumin and red blood cells (10.6%). Metabolism and Elimination
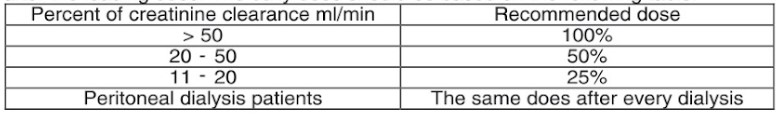
The absorbed portion of Miconazole Oral Gel is largely metabolized; less than 1% of the administered dose is excreted unchanged in the urine. The terminal plasma half-life is 20- 25 hours in most patients. The elimination half-life of Miconazole is similar in any renal impaired patient. Plasma concentrations of Miconazole are moderately reduced (approximately 50%) during hemodialysis.
INDICATIONS:
MECOZALEN oral gel is indicated in the management of fungal infections of the oral cavity and gastro-intestinal tract in adults and pediatric patients 4 months and older.
Miconazole is effective against some gram-positive bacteria in adults and paediatric patients 4 months and older, including Streptococcus pyrogenes, Staphylococcus aureus and Erysipelothrix.
CONTRAINDICATIONS:
MECOZALEN Oral Gel is contraindicated in the following situations:
– In patients with a known hypersensitivity to miconazole or to any of the other ingredients of the gel or other imidazole derivatives.
– In infants less than 6 months of age or in those whose swallowing reflex is not yet sufficiently developed.
-In patients with liver dysfunction.
-Co-administrating of the following drugs that are subject to metabolism by CYP3A4:
- Substrates known to prolong the QT-interval eg. Astemizole, bepridil, cisapride, dofetilide, halofantrine, mizolastine, pimozide, quinidine, sertindole and terfenadine. Ergot alkaloids.
o HMG-CoA reductase inhibitors such as simvastatin and lovastatin.
o Triazolam and oral midazolam.
WARNINGS AND PRECAUTIONS:
Miconazole is systemically absorbed and is known to inhibit CYP2C9 and CYP3A4 which can lead to prolonged effects of warfarin. Bleeding events, some with fatal outcomes have been reported with concurrent use of miconazole oral gel and warfarin.
If the concomitant use of MECOZALEN oral gel and anticoagulants such as warfarin is envisaged, the anticoagulant effect should be carefully monitored and titrated.
It is advisable to monitor miconazole and phenytoin levels, if they are used concomitantly.
In patients using certain oral hypoglycemic such as sulfonylureas, an enhanced therapeutic effect leading to hypoglycemia may occur during concomitant treatment with miconazole and appropriate measures should be considered.
Patients should be advised that if they experience unexpected bleeding or bruising, nosebleeds, coughing up blood, blood in the urine, black tarry stools or coffee ground vomit, to stop treatment with miconazole and seek medical advice. Severe hypersensitivity reactions, including anaphylaxis and angioedema, have been reported during treatment with miconazole formulations. If a reaction suggesting hypersensitivity or irritation should occur, the treatment should be discontinued.
Serious skin reactions (e.g. Toxic epidermal necrolysis and Stevens-Johnson syndrome) have been reported in patients receiving Miconazole Oral Gel. It is recommended that patients be informed about the signs of serious skin reactions, and that use of Miconazole Oral Gel be discontinued at the first appearance of skin rash.
It is important to take into consideration the variability of the maturation of the swallowing reflex in infants, especially when giving Miconazole Oral gel to infants between the ages of 4-6 months.
The lower age limit should be increased to 5 – 6 months of age for infants who are pre-term, or infants exhibiting slow neuromuscular development
Pregnancy and lactation: Safety in human pregnancy has not been established and the drug should not be used in pregnant women unless considered absolutely essential by the physician. The potential hazards should be balanced against the possible benefits.
It is not known whether Miconazole or its metabolites are excreted in human milk. Caution should be exercised when prescribing Miconazole Oral Gel to nursing mothers
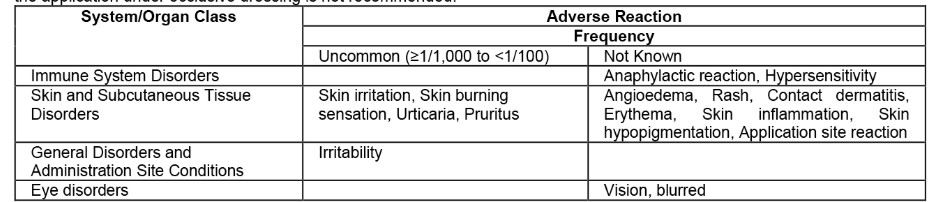
ADVERSE EFFECTS
Increases in INR and bleeding events such as epistaxis, contusion, haematuria, melaena, haematemesis, haematoma and haemorrhages have been reported in patieints treated with oral anticoagulants such as warfarin in association with Miconazole oral gel.
Common: Dry mouth, Nausea, Oral discomfort, Vomiting, Regurgitation, and Product taste abnormal.
Uncommon: Dysgeusia.
Not Known: Anaphylactic reaction, Hypersensitivity, Choking, Diarrhoea, Stomatitis, Tongue discolouration, Hepatitis, Angioedema, Toxic epidermal necrolysis, Stevens-Johnson syndrome, Urticaria, Rash, Acute generalized exanthematous pustulosis, drug reaction with eosinophilia and systemic symptoms.
INTERACTIONS:
When using any concomitant medication, consult the corresponding label for information on the route of metabolism. Miconazole can inhibit the metabolism of drugs metabolised by the CYP3A4 and CYP2C9 enzyme systems. This can result in an increase and/or prolongation of their effects, including adverse effects.
Oral miconazole is contraindicated with the coadministration of the following drugs that are subject to metabolism by CYP3A4 and CYP2C9:
– Substrates known to prolong the QT-interval for example, astemizole, cisapride, dofetilide, mizolastine, pimozide, quinidine, sertindole and terfenadine
– Ergot alkaloids
– HMG-CoA reductase inhibitors such as simvastatin and lovastatin
– Triazolam and oral midazolam.
Co-administration with warfarin is contraindicated except when oral miconazole gel is specifically prescribed and used under medical supervision with close monitoring of INR.
When coadministered with oral Miconazole the following drugs must be used with caution because of a possible increase or prolongation of the therapeutic outcome and/or adverse events. If necessary, reduce their dosage and, where appropriate, monitor plasma levels:
- Drugs subject to metabolism by CYP2C9.
- Oral hypoglycaemics such as sulphonylureas
- Other drugs subject to metabolism by CYP3A4.
- HIV protease inhibitors such as saquinavir.
- Phenytoin.
- Certain antineoplastic agents such as vinca alkaloids, bulsulfan and docetaxel.
- Certain calcium channel blockers such as dihydropyridines and verapamil
- Certain immunosuppressive agents: cyclosporin, tacrolimus, sirolimus (rapamycin).
- Others: carbamazepine, cilostazol, disopyramide, buspirone, alfentanil, sildenafil, alprazolam, brotizolam, midazolam IV, rifabutin, methylprednisolone, trimetrexate, ebastine and reboxetine. DOSE AND ADMINISTRATION:
Oropharyngeal candidosis:
One measuring spoon (provided) is equivalent to 124 mg miconazole per 5 mL gel. For infants (6-24 months):
One quarter (1/4) of a measuring spoon* of gel four times daily after meals. Each dose should be divided into smaller portions and the gel should be applied to the affected area(s) with a clean finger. The gel should not be applied to the back of the throat due to possible choking. The gel should not be swallowed immediately, but kept in the mouth as long as possible.
Adults and Children: (2 years of age and older):
2.5 mL (1/2) a measuring spoon* of gel four times daily. After meals. The gel should not be swallowed immediately, but kept in the mouth as long as possible.
The treatment should be continued for at least a week after the symptoms have disappeared.
For oral candidosis, dental prostheses should be removed at night and brushed with the gel.
Gastrointestinal tract candidosis:
The gel may be used for infants (≥4 months of age), children and adults who have difficulty swallowing tablets. The dosage is 20 mg per kg body weight per day, administered in four individual doses. The daily dose should not exceed 250 mg (10 mL oral gel) four times a day. The treatment should be continued for at least a week after the symptoms have disappeared.
OVERDOSE:
Symptoms: In the event of accidental overdose, vomiting and diarrhea may occur. Treatment: Treatment is symptomatic and supportive. A specific antidote is not available.
STORAGE CONDITIONS:
-Store at temperature below 25 °C. – Keep out of reach of children.
PACKAGING: Aluminum tube contains 50 g MECOZALEN oral gel/carton box, with measured spoonful.